Sharing is caring!
Type 1 Diabetes in Children
June 24, 2019, is a date that will forever impact our family. We go through life with many important dates, birthdays, anniversaries, graduations, etc. You never anticipate adding the day your child is diagnosed with a lifelong, chronic, and potentially deadly condition. June 24, 2019, is the day my 8-year-old daughter, the girl that made me a mama, was diagnosed with Type 1 Diabetes.
Emma finished up the 2nd grade in May 2019. A couple of weeks before the end of the school year, she fell off of our swing set and ended up with a hairline fracture in her wrist. It healed, and we all went on with our days, anticipating summer. This was the first summer she and my middle daughter would have a nanny at our home rather than do the summer program at the daycare center we have used. In true mom fashion, I had signed the girls up for swim lessons right away, and they started the first week out of school. If you remember, it was a chilly start to the summer!
Almost immediately, Emma would come home from swim lessons and usually a trip to the park with our nanny, and she would nap for a while. My husband mentioned it to me, but I blew it off as her being exhausted from all of the summer fun she was having! She will get used to it, she’s just tired! But it didn’t. I was away for the weekend, and my husband kept reporting about how lethargic Emma was acting, but she had no fever, had a terrific appetite, but just wanted to lay around, and sleep. I still thought, maybe it’s a summer cold. It was chilly at the pool, she probably just picked up a virus. She’ll get her energy back.
Her lethargy persisted. Then her emotions started to derail. My normally pretty even-tempered 8 years old started to have wild mood swings, temper tantrums in the grocery store, crying over literally nothing. I remember talking to my friend, who has an 8-year-old, asking her if she was experiencing the same thing. She agreed enough for me to think it was just some age-appropriate, pre-teen hormone shifts. But also started to trigger something more in my mind. Maybe she wasn’t transitioning to the nanny well? Maybe she missed her friends at the daycare? Maybe she and her sister are fighting too much? Maybe I need to take her to talk to someone?
We were about 2 weeks into summer when I really began to notice that some of Emma’s clothes were really loose. Had she lost weight? I put her on our bathroom scale, and I remember thinking that seemed way less than when we had the follow up for her wrist. She was set to spend the following week with my parents, and it was about this point that diabetes popped into my head, which I would quickly push aside. See, Emma wasn’t drinking a ton or using the bathroom a ton. That I thought was abnormal, anyway. That is the “classic” sign of diabetes, and she wasn’t showing it, or at least I was in denial that she was. I called our doctor’s office, just to be certain. They had her last weight recorded, and yes, she had lost weight, but not enough to be concerning at that point. And yes, lethargy and mood swings, but it’s the start of summer, so maybe she’s just really tired. All of my thoughts (denials) were confirmed. Call us back if she isn’t better in a week or two!
During her stay with my parents, I was texting my mom 2-3 times a day asking how Emma was. That was the point when the thirst and urination were much more obvious. My mom said she was really thirsty, all the time. That was pretty much what I needed to hear to schedule an appointment for as soon as she got home. The weekend Emma returned home, we started to really see her health decline. She was so lethargic, moody, and we started to notice her breathing was labored and shallow. We took her in as soon as we could on Monday, June 24th.
It was there our doctor gave us one sliver of hope, as he waited for blood and urine testing. He didn’t immediately think about diabetes and wanted to run a couple of additional tests. That is until he got her blood and urine. Emma had a blood sugar over 450, large ketones in her urine, and was not only now a Type 1 Diabetic, but was in DKA (diabetic ketoacidosis). Her body was shutting down because her pancreas was no longer producing insulin to carry all of that sugar to her cells. She was severely dehydrated. Which for how much she would drink is so ironic. Her breathing was labored because her body was trying so hard to reverse the acidosis and increase the oxygen in her system. She was so very sick.

We were sent straight to Blank Children’s ER from our doctor’s office, which thankfully is downtown. Emma was admitted immediately, and the nurses and staff went straight to work to get her on IV. Because of the severity of her dehydration, they had so much difficulty inserting a needle, and Emma experienced so much pain. It was a difficult experience as parents to watch. Emma spent that night, and the following 2 days in Blank PICU, and one day on the children’s floor. They reversed her DKA with insulin and fluids. Then they educated us about parenting a child with Type 1 Diabetes.
Emma’s pancreas no longer produces any insulin, so she is insulin-dependent for the rest of her life. That is a daunting phrase to ruminate on at 3 am, watching your child sleep in the hospital. As her parents, we are responsible for administers the right amount of insulin at the right time, so her blood sugars don’t go too high or too low. I’m forever thankful that my husband and I had a strong grasp on counting macros in our meals because we now know carb counts for many, many, many of our favorite foods. We go no where without Emma’s “kit” that includes insulin, her PDM (personal diabetes manager) device for her pump, glucose gummies or tablets for low blood sugars, usually a couple of juice boxes, maybe some fruit snacks, glucagon in case she crashes and goes unconscious and we have to take major action to save her life, her medical alert bracelet so a first responder knows she’s insulin-dependent in case of an emergency, a glucose meter, just in case her CGM (continuous glucose monitor) fails, or to double-check a high or low blood sugar.

If Emma’s behavior begins to falter from the “norm”, the first thing we utter is “What’s your blood sugar?” When she’s high, the emotional outburst, temper tantrums, and attitude pop back up. When she’s low, she’s goofy, giggly, almost like a little drunk person. And we have to make the best choice at that moment for how to treat her blood sugar. Activity, sleep, illness, travel, weather, time change, and obviously food ALL impact Emma’s blood sugars. We learn something new every single day.
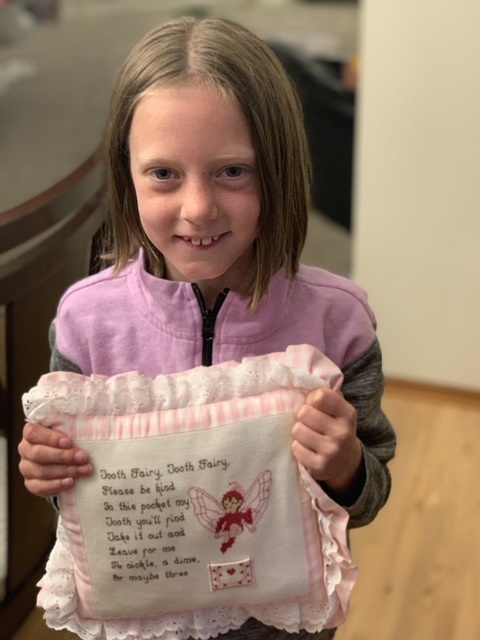
Above all of this, Emma is THRIVING!
She bounced back from her DKA and the hospital stay so quickly. She has taken ownership of her new lifestyle (I try my hardest to avoid calling it a disease or condition) and we encourage her every day that she can still do anything she wants, be anything she wants, and yes, eat anything she wants (as long as there’s insulin to cover it!). The only thing we want for Emma is to have as normal of childhood, and life, and we dreamed for her to have prior to June 24, 2019. And we know that she will!

Know the signs of Type 1 Diabetes
- Extreme thirst Frequent Urination
- Excessive Hunger
- Blurred Vision
- Extreme Tiredness
- Mood Changes
- Slow to heal from cuts/bruises
- Nausea
- Vomiting
- Sweet/Acetone smelling breath
Resources for Diabetes
November is National Diabetes Awareness Month, and November 14, 2019, is World Diabetes Day. We encourage you to wear blue on Fridays during November, and on November 14th, to stand with and support those living with Type 1 Diabetes.
About the Author

Jennifer Thompson is a wife, mom, and family wellness chiropractor serving the Des Moines community. Jennifer has been practicing in Windsor Heights for 11 years and focuses on pediatric and prenatal chiropractic care. Jennifer is married to her husband, Brian, and they just celebrated their 10 year anniversary! They have 3 daughters, Emma, age 9, Lucy, age 6, and Vada, age 2. As a family, Jennifer, her husband, and kids enjoy being outside and staying active.
Erin Huiatt
Erin is a reliable resource and stepping stone for women and families to find support and make connections within our community. She wants families to feel confident to reach out and ask for help and advice to get pointed in the right direction. She enjoys traveling and exploring with her two children in tow!





what are the root cause of type 1 diabetes and what are the solutions and their treatments?
Thank you so much for posting your story! My 7 year old son was diagnosed last week and it’s so encouraging to read other’s experiences! Thankfully, we caught it very early (we went to the pediatrician for bed wetting) and didn’t he have any ketones when he was admitted. Again, thank you for sharing!